TEVAR is a minimally invasive endovascular procedure recommended to treat thoracic aortic dissection, aortic aneurysms, and aortic ulcers. Using a stent to support the weakened aorta and bypass blood flow, the procedure provides a lower risk alternative to open-heart surgery. A new type of unibody stent has now been developed to minimise the need for future intervention.
What is the TEVAR procedure?
TEVAR (Thoracic EndoVascular Aortic Repair) is the recommended minimally invasive treatment for a dissected or aneurysmatic thoracic aorta.
The procedure involves directing a stent graft to the diseased section of aorta via an incision in the femoral artery. It scaffolds the aorta from within and allows blood to be redirected down the true lumen, removing pressure from the damaged or dissected layers of the aorta.
However, when an ulcer, aneurysm or dissection occurs in the distal aortic arch or near the left subclavian artery, a single TEVAR stent is not sufficient. An additional stent is then also required to protect and preserve the left subclavian and left vertebral artery.
Previously, a separate vascular bypass (carotid to subclavian) or two stents were used in such cases – one for the left subclavian artery, and one for the descending aorta which required support. However, stents are not guaranteed to stay in place and in 10-15% of cases they move from their original position, resulting in an endoleak (when blood leaks out from in between two stents placed together side-by-side). In these cases, further intervention may be required to correct the endoleak and prevent further complications or rupture. By using a new unibody stent graft with an additional branch sewn in for the left subclavian artery, this risk is completely eliminated.
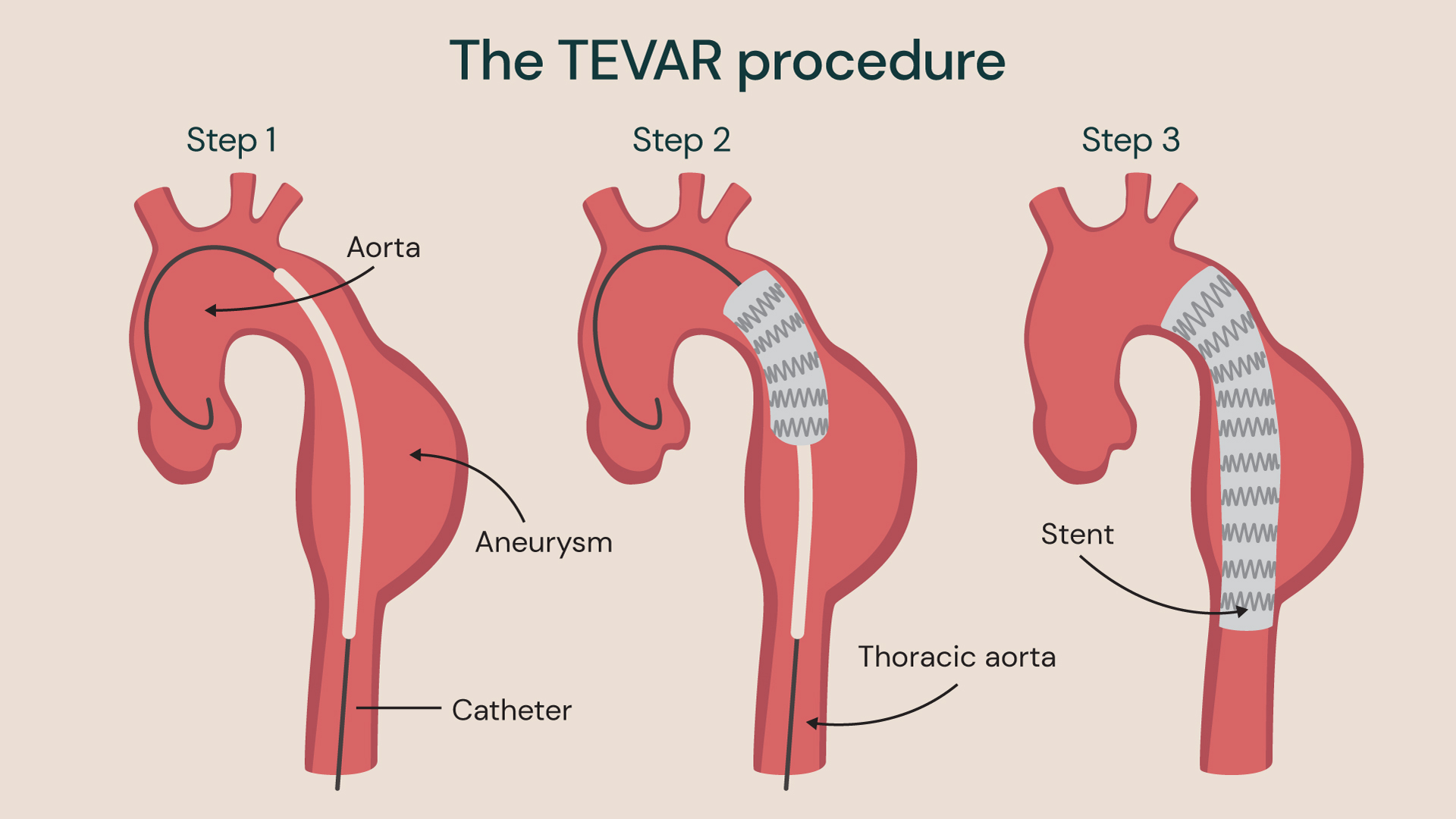
Standard TEVAR procedure for aortic aneurysm using one stent to support the aorta
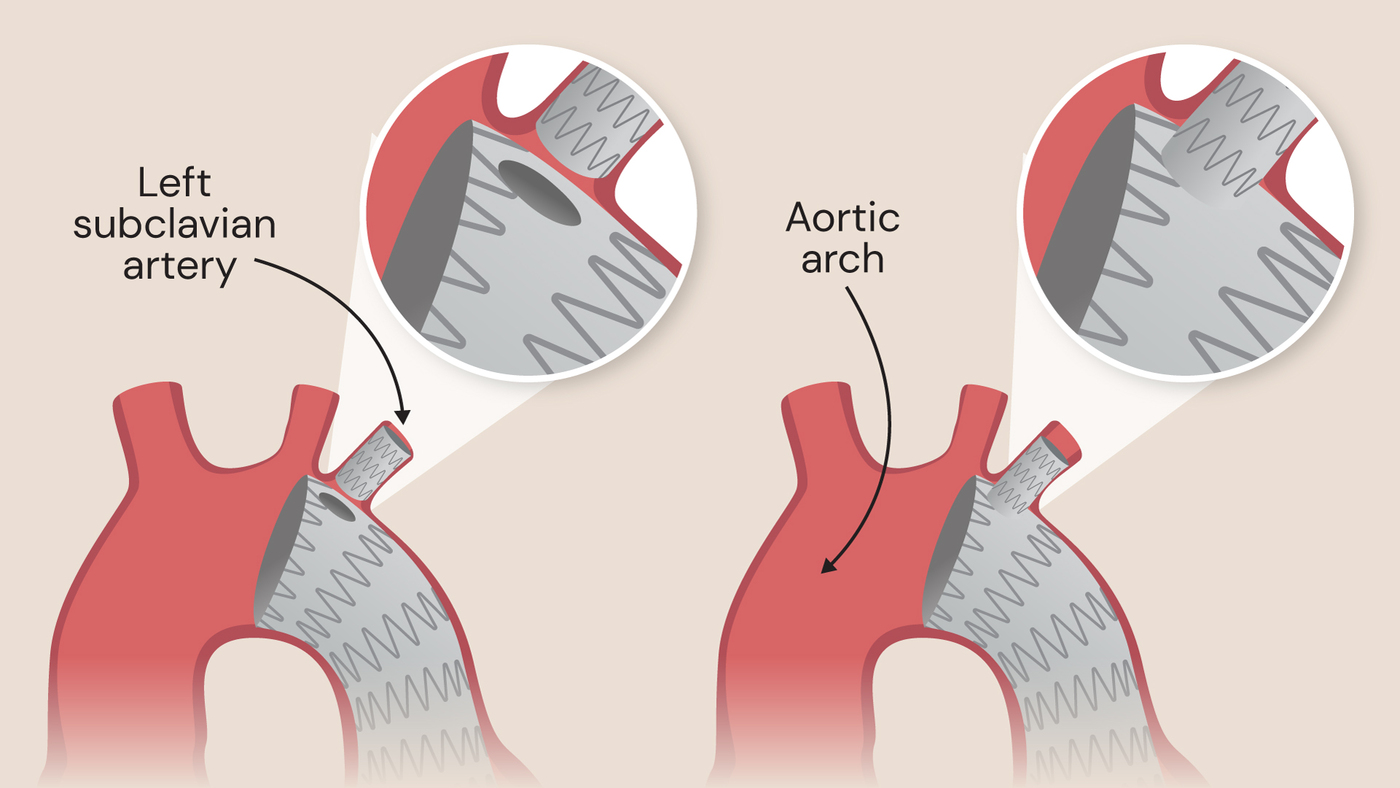
Standard separate side branch (left) and unibody side branch device (right)
What is a unibody stent graft?
“The beauty of the unibody device is that it combines the main body for the aorta with an attached side branch,” explains Prof Nienaber. “The side branch of the unibody stent is placed into the left subclavian artery, preserving antegrade flow to the left arm and vertebral artery, while also avoiding the need for a vascular bypass between the left carotid and the left subclavian artery.”
Further to this, the fact that the stent is in one piece means that there is no risk of endoleak between multiple stent parts. The need for further intervention to connect the stent to the left subclavian circulation is also removed.
The procedure is performed under general anaesthetic in around 90 minutes, and recovery time is two to three days for a fit patient. However, most patients with aortic disease are in their 70s or 80s, and therefore may require around five days of recovery.
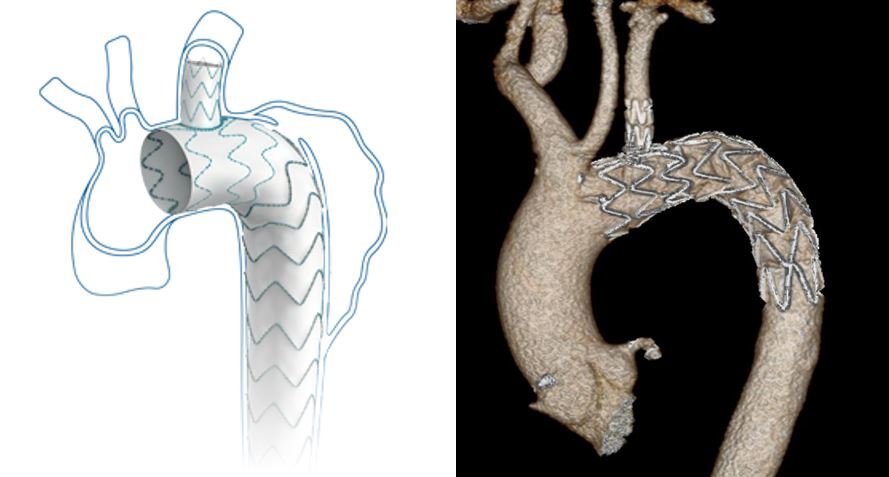
The manufacturer’s diagram of the unibody stent, and a scan depicting the stent in place in a patient’s aortic arch
Custom made stents for personalised care
Before the TEVAR procedure takes place, the patient undergoes an ECG-gated CT scan to produce a high-quality image of their anatomy, which essentially acts as the blueprint for building and manufacturing the unibody stent device.
“The stent will vary in terms of length, width and diameter,” explains Prof Nienaber, “so the device must be tailored and fitted to the individual anatomy of the patient.” Once the scans have been carried out, it typically takes 10-14 days for the stent to be made.
The device itself consists of a scaffold structure made from nitinol, an alloy with temperature memory. It expands to its full extent at the temperature of 37 degrees, meaning that it can be passed through the femoral artery, before fully expanding once placed inside the aorta at body temperature.
The stent is essentially a tube made from a biocompatible mesh, with some surrounding fabric, which supports the true lumen of the aorta and, in cases of aortic dissection, seals all communication to the false lumen. This also reduces systolic pressure in the blood stream, preventing the pressure from being transposed onto the aortic wall.
Case study: Patient receives unibody stent in a UK first
A 70-year-old patient was treated at the Royal Brompton Hospital in January in a UK first procedure. Diagnosed with an aortic ulcer in 2021, the patient was monitored by our cardiology team with regular CT scans at six monthly intervals.
In December 2022, the patient had a fourth CT scan which revealed that the ulcer had doubled in depth and had increased by a third in width (the threshold size for intervention is 20mm in width or 10mm in depth) and therefore required urgent treatment. Prior to the procedure, the patient sought advice from his medical contacts, who recommended Prof Nienaber and the team at the Royal Brompton for their expertise in the field.
The patient’s ulcer had grown in the aortic arch, very close to the left subclavian artery. “The unibody device has the inbuilt side branch for the left subclavian artery,” explains Prof Nienaber, “which allowed us to place an endograft into the descending thoracic aorta and the arch to avoid rupture of the ulcer and simultaneously preserve his left subclavian artery without surgery.”
The procedure was a huge success, and the patient was discharged from the Royal Brompton after only five days. Within two weeks, he had resumed his active lifestyle and was back to lifting weights.
Looking ahead
This ground-breaking procedure with the unibody stent is a significant development in the field of TEVAR, offering new hope for patients looking for an alternative to carotid to left subclavian bypass surgery in the neck. The use of minimally invasive surgery and custom-designed unibody stents represents a major step forward in the treatment of aortic ulcers, aneurysms and dissections.
When to refer to us
Patients who have been diagnosed with aortic ulcers, aneurysms or type B dissection should receive regular monitoring to track the size of the pathology and assess any growth or change, and can be referred for this.
Our multidisciplinary aortic team is happy to consult, diagnose or treat and survey patients with various known aortic conditions, as well as design personalised surveillance plans for future years.
Contact our customer services team to learn more about TEVAR, stent options, and our aortic care services.
Related content
-
Aortic aneurysm
Aortic aneurysm occurs when a part of the aorta becomes weak and becomes enlarged.
-
Aortic disease
Aortic stenosis is a narrowing of the aortic valve opening, restricting blood flow to the aorta.
-
Aortic dissection
Aortic dissection is when the aorta tears causing blood to rush through.
-
FLIRT (False Lumen Intervention to Promote Remodelling and Thrombosis)
Although the vast majority of TEVAR procedures are very successful, 2% of patients may require reintervention. For this, our cardiology experts developed FLIRT.
-
Thoracic endovascular aortic repair (TEVAR) procedure
TEVAR uses a stent-graft to reinforce and repair a weakened section of the aorta.

